In hospital emergency departments, seconds can mean the difference between life and death. Delays in triage and care can lead to catastrophic outcomes for patients and for healthcare providers. ERTriage offers a transformative solution, harnessing advanced technology to optimize emergency care, save lives, and improve hospital operations.
The Need for ERTriage in Hospitals
Emergency departments face relentless challenges, including high patient volumes, resource shortages, and complex case prioritization. These hurdles often result in delayed care, which can lead to avoidable deaths, overcrowded departments, and overburdened staff.
ERTriage addresses these pain points head-on by:
- Enhancing patient prioritization through AI-powered systems.
- Reducing wait times for critical care.
- Improving resource allocation to manage capacity more effectively.
How ERTriage Revolutionizes Emergency Care
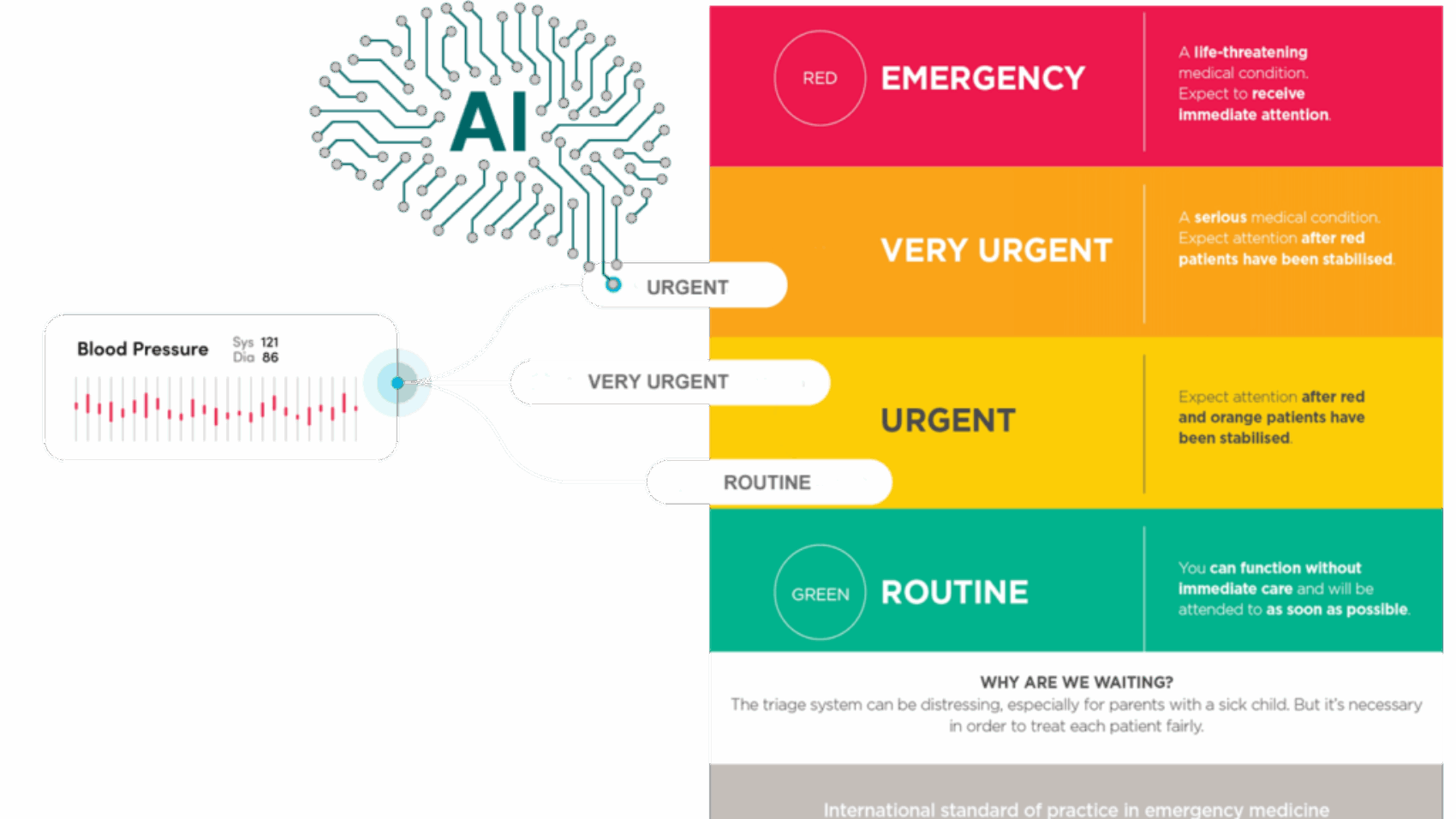
- AI-Powered Triage for Accurate Prioritization
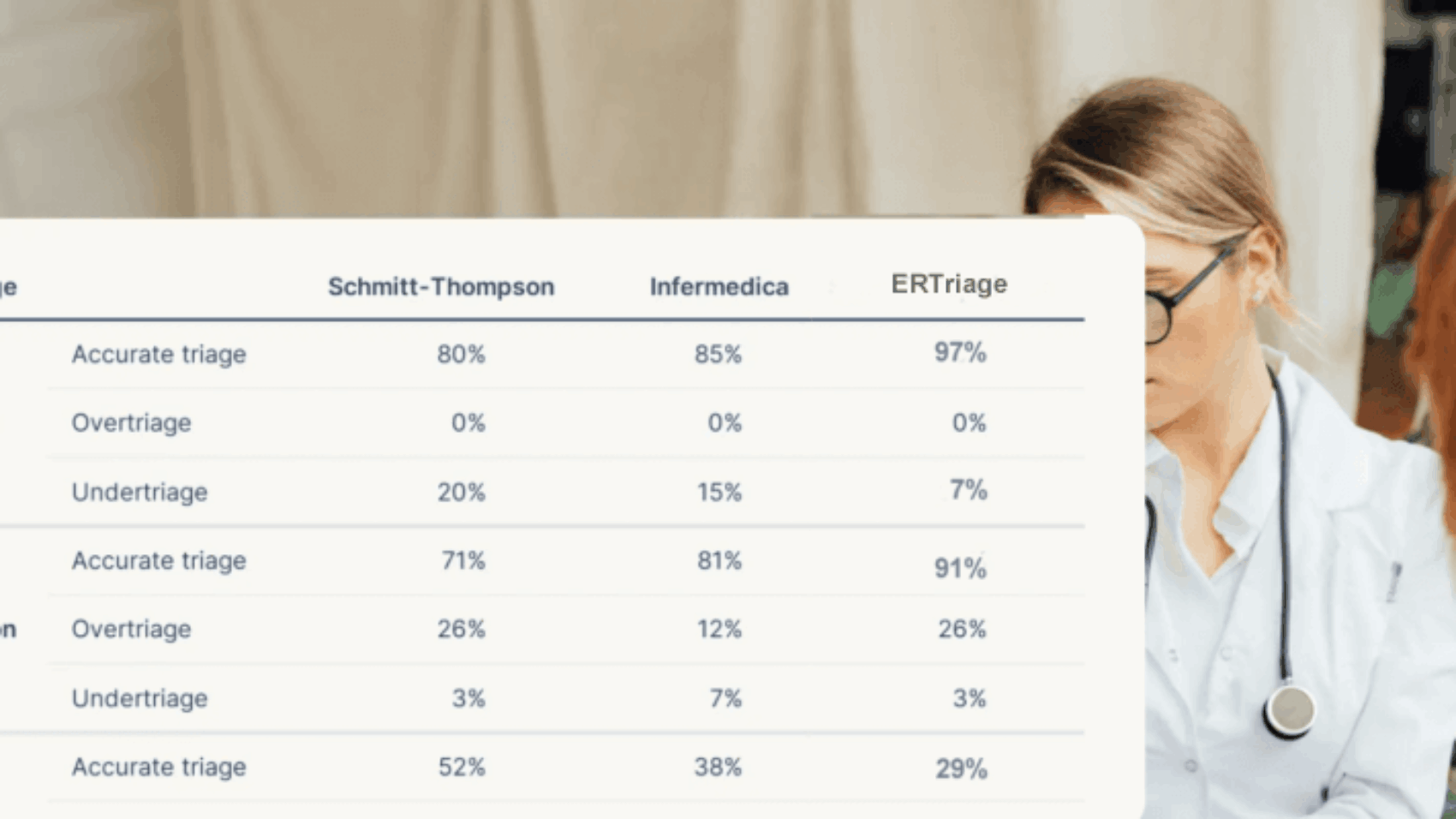
ERTriage uses cutting-edge algorithms to analyze patient data in real-time. It assesses symptoms, vital signs, and medical history to rank cases by urgency. This ensures patients with life-threatening conditions are seen promptly while non-critical cases are appropriately managed. - Streamlined Workflow Integration
Designed to seamlessly integrate with existing hospital systems, ERTriage optimizes workflows. By automating routine tasks and enhancing communication between departments, it reduces bottlenecks and keeps the emergency department running smoothly. - Real-Time Monitoring and Alerts
ERTriage enables continuous patient monitoring, providing alerts for changes in condition. This ensures that deteriorating cases are flagged immediately, allowing for timely intervention.
Benefits of ERTriage for Hospitals
- Life-Saving Efficiency
By prioritizing patients accurately, ERTriage reduces delays in treatment, lowering mortality rates and improving recovery outcomes. - Enhanced Reputation
Hospitals that adopt ERTriage demonstrate a commitment to cutting-edge care, attracting patients and building trust within the community. - Resource Optimization
ERTriage minimizes waste by directing resources where they are needed most. This includes staff time, medical supplies, and physical space. - Improved Staff Well-Being
With reduced pressure and better workflows, hospital staff experience less burnout, leading to higher morale and retention rates.
Why ERTriage is a Must-Have for Hospitals
The adoption of ERTriage is more than just a technological upgrade—it’s a strategic decision with long-term benefits. Hospitals face growing demands for efficiency, patient safety, and financial sustainability. ERTriage meets these needs by delivering:
- Faster care for critical cases.
- Improved patient satisfaction and outcomes.
- Data-driven insights for continuous improvement.
How ERTriage Benefits Healthcare Providers
ERTriage enhances the efficiency and effectiveness of healthcare providers, particularly in emergency settings. By automating patient triage with AI, ERTriage helps healthcare providers quickly prioritize critical cases, reducing delays in treatment. Real-time monitoring alerts providers to any changes in patient conditions, allowing for immediate action. With streamlined workflows, healthcare providers spend less time on administrative tasks and more time on patient care. This leads to improved job satisfaction, reduced burnout, and a more manageable work environment. ERTriage empowers healthcare providers to deliver timely, life-saving care with confidence and efficiency.
Conclusion
Hospitals must rise to the challenge of delivering faster, safer, and more efficient emergency care. ERTriage provides the tools to meet these demands, transforming emergency departments into high-performing, patient-centered systems.
Contact with us today to learn how ERTriage by Carepoi can help save lives, optimize resources, and secure your hospital’s place at the forefront of modern healthcare.